Acute and chronic tonsillitis: what kind of disease it is and how to treat it. Symptoms of tonsillitis, treatment and prevention Tonsillitis disease symptoms
Almost everyone has encountered such a problem as a sore throat during a cold. The tonsils enlarge, become swollen and red - this is quite normal in this condition, but there are cases when their inflammation develops against the background of complete health. In this case, doctors make a diagnosis: What kind of disease is this? Let's try to figure it out in our article. Some underestimate the seriousness of the problem, but in vain.
Essence of the disease
Everyone has tonsils in their throats, which can be affected by the inflammatory process. If the inflammation is almost constant, then it is said that chronic tonsillitis occurs. ICD 10 includes it, as well as the acute form of the disease, into independent forms that have their own code:
- Code J03.
- J35.0.
Assigning your own codes to diseases makes it easier to maintain statistics and dispensary records of patients.
The development of chronic inflammation occurs under the influence of many forms of microorganisms, which a healthy person almost always has. But a number of factors provoke their mass reproduction, which leads to an exacerbation of the disease.
In a person’s throat there is a lymphopharyngeal ring, which includes 7 tonsils, but it is the palatine tonsils that most often become inflamed.
The tonsils are a lymphoid organ that actively provides immunobiological protection to the body. Periodic inflammatory processes lead to the formation of immunity; this function is especially active in children.
Quite often, a sore throat is a companion to colds, in which case they say that acute tonsillitis occurs. It proceeds a little more mildly, does not have such pronounced symptoms, but most often develops due to poorly treated sore throat.
Mild symptoms are not a reason to delay treatment. Chronic tonsillitis and inflammation of the pharyngeal mucosa) can lead to serious complications, which will be discussed below.
For what reason does the disease develop?
Otolaryngologists often claim that almost the entire population suffers from chronic tonsillitis. In a sense, we can agree with this, because every person’s tonsils contain a huge number of bacteria, but if the body is completely healthy, then it does not allow pathogenic microorganisms to multiply and quickly suppresses their growth, but in the presence of an inflammatory process or a weakened immune system, this can be done it doesn't work.
The disease chronic tonsillitis does not form immediately, it all starts with the acute phase, it can become chronic for the following reasons:
- Poorly treated tonsillitis is one of the main reasons for the development of chronic tonsillitis. Most of us, as soon as the sore throat subsides and the temperature subsides, we stop taking medications and antibiotics, and this is a big mistake. Chronic tonsillitis and pharyngitis recede, but do not give up their positions completely, so they will soon return again.
- Persistent pharyngitis, which many simply do not pay attention to and believe that no special treatment is required, will certainly lead to the development of a chronic form of the disease.
- Failure to maintain oral hygiene and the disgusting condition of teeth will certainly cause the development of chronic tonsillitis. The constant presence of pathogenic microflora in the oral cavity will lead to this.
- A chronic form of rhinitis or periodically worsening allergic rhinitis can result in tonsillitis.
- Prolonged disruption of nasal breathing can lead to the development of chronic tonsillitis. Many people have no idea that this is connected, for example, with adenoids. A deviated nasal septum and polyps can also cause this.
As can be seen from the above, many reasons can provoke the development of a disease that must be treated.
Types of chronic tonsillitis
To answer the question of how to cure chronic tonsillitis once and for all, it is necessary to understand that it can manifest itself in different ways. Doctors note two scenarios:
- After treatment, tonsillitis subsides a little and it seems that we managed to get rid of it, but as soon as you get a little cold or get your feet wet, it’s right there.
- In the second option, the inflammatory process does not stop, it may subside a little, the patient even feels quite tolerable, goes to work, but the doctor notes that not everything is in order.
Both options require medical intervention to select effective measures to combat this disease.
In medical circles, there are two forms of chronic tonsillitis:
- Compensated. It manifests itself as a slight inflammation of the tonsils, sore throat, the general condition of the patient is normal. Doctors say in such cases that the tonsils compensate for the state of inflammation and generally cope with their function.
- The decompensated form of chronic tonsillitis usually manifests itself not only as pain in the throat, sore throat develops, and other organs are also involved in the process.
Any form of tonsillitis can lead to infection of the entire body, so do not delay a visit to an ENT doctor.
Symptoms of chronic tonsillitis
If there is chronic tonsillitis, then such patients may often complain of an unreasonable sore throat, which occurs not only when swallowing, but also during yawning. Painful sensations may appear after eating ice cream or drinking a cold drink, which is not uncommon in the summer; it turns out that this is how a person himself provokes an exacerbation of tonsillitis.
If chronic tonsillitis occurs, the following symptoms usually appear:

When all of the listed signs appear, patients try to get rid of them as quickly as possible, but it is more important to find out the reason that provoked the inflammatory process. This can only be done by a competent specialist who recognizes chronic tonsillitis. How to get rid of this disease forever and without complications is a question that should be asked specifically to the doctor.
Making a diagnosis
Making the correct diagnosis in the presence of chronic tonsillitis is not at all easy. The doctor first examines the patient and listens to his complaints. The patient's medical history is also studied. Next, the doctor palpates the lymph nodes and examines the tonsils.

This does not end there, as the symptoms may resemble other diseases. Therefore, the doctor will definitely take discharge from the lacunae for analysis. If the purulent discharge has an unpleasant odor and a mucous structure, then most likely the patient has chronic tonsillitis. That this is exactly this disease can be concluded based on a whole complex of symptoms and signs.
To clarify the diagnosis, the doctor will pay attention to the general condition of the patient’s body and any deviations from the norm. In the presence of a chronic form of tonsillitis, the edges of the palatine arches will be thickened, and scar adhesions between the tonsils and arches will be visible. The tonsils themselves have a loose appearance, with purulent plugs or discharge in the lacunae.
Additional blood tests for antibodies to streptococcus may be required. Only after the diagnosis of chronic tonsillitis is confirmed, the doctor can prescribe the necessary treatment.
Therapy for chronic tonsillitis
To get rid of the chronic form of the disease you will have to try hard. Doctors, as a rule, recommend comprehensive treatment; this is the only way to ease your chronic tonsillitis symptoms:
- Local treatment (the photo demonstrates this) is one of the first to be prescribed. To do this, rinse with medicinal solutions and herbal infusions.

- During this procedure, purulent plugs are washed out. To carry it out, antibacterial and disinfectant solutions are used, for example, Furacilin, Miramistin, Chlorhexidine.
- Antibacterial therapy, which consists of taking antibiotics that are selected taking into account the sensitivity of the microflora.
- Physiotherapeutic procedures.
- Removal of tonsils.
The greatest effect is achieved only by complex therapy, which is preferably carried out twice a year.
Physiotherapeutic treatment
Physiotherapy is most effective during the period of remission of the disease. The following methods show the best results:
- Laser therapy. Due to its antibacterial and anti-inflammatory effects on the tonsils, this method gives excellent results.
- Application of short-wave UV radiation to the throat and oral cavity.
- Ultrasonic exposure, with which you can not only influence the source of infection, destroying the structure of the curdled mass that appears, but also irrigate the tonsils with antibacterial solutions.
- Inhalation with wet steam, but it must be remembered that at high temperatures this procedure is contraindicated. For inhalation, you can use infusions of medicinal herbs.
- Phonophoresis of vitamins also gives a good effect.
The combination of physiotherapeutic treatment methods with medications and local therapy gives good results. There is no other way to get rid of this insidious disease forever.
Surgical intervention
Sometimes, when asked how to cure chronic tonsillitis forever, some doctors recommend tonsillectomy, that is, removal of the tonsils. But it is worth remembering that there is no need to rush to get rid of them, this can lead to even more serious consequences. Although there are situations where tonsil removal is necessary, the usual indications for surgery are:
- If the disease worsens up to 4-5 times a year.
- If the inflammatory process spreads to neighboring tissues.
- There is a danger of blood poisoning.
- There are signs of damage to the kidneys or heart muscle.
As a result of the operation, the tonsils may be completely removed or only partially removed when the doctor excises the overgrown tissue.
It must be remembered that tonsillectomy has its own contraindications, these include:
- Leukemia.
- Hemophilia.
- Tuberculosis in open form.
- Heart defects.
- Nephritis and some other pathologies.
If surgery is necessary, but there are serious contraindications to its implementation, then the patient is recommended to use cryogenic therapy.
Features of the treatment of chronic tonsillitis in children
If chronic tonsillitis is detected in a child, treatment should begin immediately. Taking into account the characteristics of the child’s body, therapy should be selected carefully, especially with regard to antibacterial agents.

Conservative treatment of tonsillitis in children must begin with adherence to the correct daily routine and diet. An important factor is the implementation of hardening procedures.
Parents should, if possible, eliminate all factors that could provoke an exacerbation of the disease. The use of local remedies gives a good effect if done promptly and regularly.
Tonsils can be lubricated with Lugol, and colloidal silver can also be used. During therapy, doctors often prescribe antiallergic drugs, as an unexpected reaction of the body is possible. This is especially true for antibiotics, which must be prescribed to children carefully.
Physiotherapeutic procedures in children also give good results (laser therapy, electrophoresis, magnetic therapy).
For chronic tonsillitis in children, pediatricians often prescribe bacteriophages; therapy with their use is quite effective. But it must be borne in mind that in the acute form of the disease it is better to give preference to antibiotics.
Considering that the treatment of tonsillitis is a long process, you can think about therapy with homeopathic medicines. Many parents leave good reviews about Vokara. It should be taken 1 drop per year of the child’s life, first diluted in water. Frequency of administration up to 8 times a day during exacerbation, during remission three times is enough.
When treating chronic tonsillitis in children, as well as in adults, it is important to remember that only an integrated approach to therapy can give the desired effect.
Tonsillitis in pregnant women
It is advisable to treat all existing diseases before pregnancy, but if there are chronic pathologies that make themselves felt in an interesting situation, then therapy should not be postponed. requires treatment, but only under the strict supervision of a doctor.
Considering the interesting position of the woman, the doctor may prescribe procedures such as:
- Treatment of tonsils with antiseptic compounds.
- In a specialist’s office, a woman’s throat and tonsils are washed with special medications.
- At home, it is recommended to gargle with infusions of medicinal herbs.
- Sprays and lozenges are prescribed.
A pregnant woman is prohibited from taking many medications, so it is very important to follow a daily routine, proper nutrition, and more vitamin supplements. If an exacerbation of the disease occurs during pregnancy, it is recommended:
- Often gargle with a solution of salt, soda and a few drops of iodine.
- Do inhalations with medicinal herbs, for example, sage.
- A warm drink with honey and lemon is recommended.
- To wipe the tonsils, you can use Chlorophyllipt or propolis tincture.
- At elevated temperatures, you can take a Paracetamol tablet.

During pregnancy, the most important thing when treating chronic tonsillitis is not to harm the baby, so all remedies should be selected only by the attending physician.
If you do not take this pathology very seriously, then tonsillitis can even provoke congenital defects in the baby, and in serious cases, pregnancy failure and miscarriages.
Traditional medicine for the treatment of chronic tonsillitis
If there is chronic tonsillitis, treatment with traditional methods gives good results in combination with drug therapy. It is necessary to take into account that treatment should be carried out long-term and regularly. Traditional healers advise using the following recipes for rinsing:
- Infuse 2 tbsp. l. dry yarrow in 200 ml of boiling water. Use the infusion warm several times a day.
- Dissolve 3-4 drops of basil oil in a glass of boiled water and gargle with the mixture.
- Prepare a mixture of 1 tbsp. spoons of linden flowers, 2 spoons of oak bark, 3 spoons of chamomile and pour it all with a liter of boiling water. After cooling, add a teaspoon of honey. Rinse three times a day after meals.
You can offer recipes for lubricating the tonsils:
- Mix aloe juice and honey in equal proportions and lubricate the tonsils every day for two weeks; in weeks 3 and 4, you can carry out the procedure every other day.
- To treat tonsils, you can use fir oil up to 5 times over 3 days, you can also instill 1 drop into the nose.
- For kids, a mixture of 1 part radish juice and 3 parts honey is perfect for lubricating the tonsils. At the same time, you can take a decoction of chamomile, mint, and calendula orally to generally strengthen the immune system.
There are a lot of folk recipes to alleviate the condition during an exacerbation of chronic tonsillitis, but we must remember that therapy is usually long-term.
Complications of chronic tonsillitis
If tonsillitis itself is an unpleasant disease, but generally not dangerous, then in the absence of treatment it can have quite serious undesirable consequences. Chronic causes the following:
- Frequent sore throats become a constant companion for a person.
- This disease negatively affects the cardiovascular system.
- It also affects the digestive system, since the intestinal microflora suffers and the mucous membrane is in an inflamed state.
- The development of pyelonephritis and other kidney pathologies is not uncommon.
- Attacks of suffocation may develop.
- With chronic tonsillitis, the joints begin to suffer, and the development of rheumatism and arthritis is not far off.
- Due to this disease, depression develops.
From all that has been said, it is important to remember that a fairly serious diagnosis is “chronic tonsillitis.” That this disease definitely requires timely treatment should not raise any doubts.
Prevention
The development of the disease can be prevented by preventive measures. Among these are the following:
- Healthy lifestyle.
- Hardening procedures.

- Taking medications that strengthen the immune system, for example, drugs “Immunal”, “Imudon” and others.
If you don't allow it to escalate, it won't be scary.
The result of all that has been said can be summed up as follows: any disease needs timely treatment. Even a seemingly harmless disease can lead to serious consequences that require longer therapy. Take care of your health and treat it with a sense of responsibility.
Sluggish long-term inflammation of the tonsils- chronic tonsillitis. Its symptoms, unlike acute tonsillitis (tonsillitis), are not always obvious. Despite the locality of inflammation, chronic tonsillitis is a common disease. Its danger cannot be underestimated.
Palatine tonsils
Their meaning
Palatine tonsils(tonsillis palatinus) - tonsils or tonsils - important peripheral organ of the immune system. All tonsils - lingual, nasopharyngeal (adenoids), tubal, palatine - are lined with lymphoid and connective tissue. They form a barrier-protective lymphadenoid pharyngeal ring (Pirogov-Waldeer lymphoepithelial ring) and take an active part in the formation of local and general immunity. Their work is regulated by the nervous and endocrine systems. The tonsils have a rich blood supply, which emphasizes their high working efficiency.

The term “chronic tonsillitis” refers to chronic inflammation of the palatine tonsils, because it occurs much more often than similar inflammation of all other tonsils combined.
Pathological forms of chronic tonsillitis

Chronic tonsillitis
 Symptoms from the ENT organs
Symptoms from the ENT organs
- Tonsils:
- often enlarged, loose, spongy, uneven;
- reduced, dense, hidden behind the palatine arches.
Atrophy of the tonsils occurs in adults due to gradual scarring and replacement of the lymphoid tissue involved in inflammation with connective tissue.
- Tonsil mucosa:
- inflamed, reddish or bright red.
- Gaps:
- can be expanded, the entrance openings (mouths) are gaping.
Sometimes on the surface of the tonsils, in the mouths or through the epithelial cover, the purulent contents of the lacunae are visible - yellowish-white plugs.
- Palatine arches:
- reddish or bright red;
- edges are swollen;
The palatine arches can be fused to the tonsils.
- The angle between the anterior and posterior palatine arches is often swollen.
- When pressing on the tonsil with a spatula, purulent or caseous mucus with an unpleasant, pungent odor is released from the lacunae.
General symptoms of chronic tonsillitis
- Sore throats as repeated exacerbations of chronic tonsillitis:
- can be frequent, for the slightest reason;
- sometimes chronic tonsillitis occurs without exacerbations (nonanginal form);
- atypical sore throats - last a long time, at reduced or slightly increased body temperature, and are accompanied by severe general intoxication (headache, nausea, pain in muscles and joints).
- Regional cervical lymph nodes:
- often enlarged and painful. Enlarged jugular lymph nodes are of great diagnostic importance.
- Intoxication:
— low-grade (37 – 38 0 C) increase in body temperature in the evenings;
- “unmotivated” headache;
- nausea, digestive problems;
- lethargy, fatigue, low performance.
- Feeling of awkwardness, tingling, foreign body sensation, lump in the throat.
- Periodic sore throat, radiating to the ear or neck.
- Bad breath.
Causes of development of chronic tonsillitis
1. Decrease in general and local reactivity of the body.Physiological reactivity is the body’s ability to respond to environmental changes (infection, temperature changes, etc.) as a factor that disrupts its normal state.
The capabilities of each person’s own immunity are determined genetically and do not change throughout life. For example:
— carriers of the leukocyte antigen system (immune passport) HLA B8, DR3, A2, B12 are characterized by a strong immune response;
- for carriers of HLA B7, B18, B35 - weak.
However, the implementation of existing immune capabilities (reactivity) may vary depending on external and internal conditions.
With a negative decrease in reactivity (dysergy), external immune processes are inhibited, depressed, the protective function of the tonsils is weakened: the phagocytic activity of lymphoid cells is reduced, the production of antibodies is reduced. The weakening of local immunity in the nasopharynx is manifested by a sluggish, protracted inflammatory process with erased symptoms - chronic tonsillitis. Dysergy can also manifest itself as a perverted (atypical) reaction - an allergic inflammatory reaction.
Factors that reduce the body's reactivity:- Hypothermia.
- Fasting, hypovitaminosis, unbalanced diet:
lack of protein in food, deficiency of vitamins C, D, A, B, K, folic acid reduces the production of antibodies.
- Overheating.
- Radiation.
- Chronic poisoning by chemicals:
alcoholism, smoking, taking a number of medications, environmental or occupational exposure to toxic substances, etc.
- Diseases of the nervous system, stress syndrome:
It has been proven that high levels of ACTH, adrenaline, and cortisone in the blood inhibit the production of antibodies.
- Endocrine system diseases:
patients with uncompensated diabetes or thyroid dysfunction often suffer from suppurative processes in the tonsils.
- Violation of work and rest schedule:
Insufficient sleep, overwork, physical overload.
- An acute illness, severe surgery, or heavy blood loss lead to a temporary decrease in reactivity.
- Childhood.
Up to 12–15 years of age, a dynamic balancing occurs between the nervous and other systems of the body, the formation of an “adult” hormonal background. In such changing internal conditions, the body's reactivity is not always adequate.
- Old age.
Attenuation of general metabolism and changes in hormonal status lead to dysergy.
2. Depletion of the immune system or secondary immunodeficiency states (IDS).Local weakening of immunity in the nasopharynx and the development of symptoms of chronic tonsillitis in some cases are a consequence of secondary IDS.
Secondary immunodeficiency is an acquired decrease in the effectiveness of certain parts of the immune system. IDS causes various chronic inflammations, autoimmune, allergic and tumor diseases.
Common reasons secondary IDS:
- Protozoal diseases, helminthiases:
malaria, toxoplasmosis, ascariasis, giardiasis, enterobiasis (pinworm infection), etc.
- Chronic bacterial infections:
leprosy, tuberculosis, caries, pneumococcal and other infections.
- Persistent viruses:
viral hepatitis, herpetic (including EBV, cytomegalovirus) infections, HIV.
- Nutritional defects:
obesity, cachexia, protein, vitamin, mineral deficiency.
- General diseases, pathological processes, intoxications, tumors.
The risk of developing chronic tonsillitis and the outcome of the inflammatory process in the tonsils mainly depend on the condition of the whole organism.
IgA deficiency and chronic tonsillitis
To destroy pathogenic bacteria and viruses, lymphocytes of the tonsils produce immunoglobulin antibodies of all classes, as well as lysozyme, interferon, and interleukins.
Class A immunoglobulins (IgA) and secretory SIgA (unlike IgM, IgG, IgE and IgD) penetrate well into saliva and mucous membranes of the oral cavity. They play a decisive role in the implementation of local immunity.
Due to weakened reactivity or disruption of the biocenosis of the oropharynx, a local deficiency in IgA production occurs. This leads to chronic inflammation in the tonsils and the formation of a local focus of chronic microbial infection. Lack of IgA causes hyperproduction of IgE reagins, which are primarily responsible for the allergic reaction.
Chronic tonsillitis is an infectious-allergic disease.In an attempt to balance the production of immunoglobulins, lymphoid tissue may grow. Hyperplasia of the palatine and nasopharyngeal tonsils (adenoids) are common symptoms of chronic tonsillitis in children.
Clinical forms of chronic tonsillitis Symptoms
| HT form. Treatment tactics. | Clinical symptoms |
Simple form. Conservative treatment. |
1. Liquid pus or caseous-purulent plugs in the lacunae. |
Toxic-allergic form Conservative treatment. |
1. All symptoms are simple. |
Toxic-allergic form Tonsillectomy |
1. All symptoms of TAF I. |
In chronic tonsillitis, there are more than 30 combinations of various microorganisms in the tonsils. Pathogenic streptococci, staphylococci, viruses, fungi penetrate into the general lymph and bloodstream, poison and infect the entire body, leading to the development of complications and autoimmune diseases.
Diagnosis of chronic tonsillitis

The diagnosis is made on the basis of anamnesis, complaints of the patient and is based on a thorough, repeated examination of the tonsils in the non-acute period of the disease, checking the depth and nature of the contents of the lacunae (sometimes using special instruments).
Bacteriological examination of mucus lacunae does not have a decisive diagnostic value, because pathogenic microflora in the crypts, including hemolytic streptococcus, is often found in healthy people.
It is important to identify the condition of the jugular lymph nodes.
Treatment of chronic tonsillitis
symptomatic/local/general
The basis of conservative treatment of chronic tonsillitis is the restoration of local, general immunity and desensitization (suppression of allergic reactions) of the body. 
1. Cleansing the tissues of the palatine tonsils from pathological contents helps to form normal local reactivity.
The most effective today is considered to be a course of vacuum rinsing of the entire thickness of the tonsils using the “Tonsillor” apparatus.
Washing lacunae with antiseptic agents (furacilin, boric acid, rivanol, potassium permanganate, iodinol) according to the Belogolovov method is also used.
After cleansing the lacunae from pus and plugs, they are irrigated with mineral waters, interferon preparations, etc.
- Washing lacunae with antibiotics should be avoided due to undesirable complications (allergies, fungal infection, impaired mucosal regeneration).
- Gargling with herbal infusions or antiseptic solutions is an ineffective method of treating chronic tonsillitis.
2. An important stage in restoring local immunity is sanitation and hygiene of the oral cavity: treatment of diseased teeth (caries) and gums, cleansing the oropharynx of food debris (regular rinsing, brushing teeth after eating). Sanitation of the nasopharynx and nasal mucosa: treatment of adenoids, pharyngitis, vasomotor or allergic rhinitis; as well as sinusitis and ear diseases.
3.
Moist mucous membranes are a prerequisite for the normal occurrence of local immune reactions. Measures to combat dry nasopharynx:
— irrigation of mucous membranes with aerosol preparations of sea water, low-salt solutions;
— humidification of inhaled air: ventilation, installation of air humidifiers in heated rooms;
- moisturizing the mucous membranes naturally: drinking plenty of fluids during exacerbations of tonsillitis. During the period of remission, the drinking regime is about 2 liters of clean water per day.
4. Prescribes local/general background immunocorrection immunologist-allergist. Treatment with immunotropic drugs is carried out strictly individually, taking into account the patient’s immune and allergy status.
Absolute contraindication for the use of natural or other biostimulants:
— oncological (including benign, treated) diseases in the patient’s history;
- suspicion of a tumor process.
5.
Physiotherapy for the tonsil area:
— UV irradiation, quartz treatment;
— UHF, microwave;
- ultrasound treatment.
Physiotherapy restores local immunity, improves lymph and blood circulation in the tonsils, and improves lacunar drainage (self-cleaning).
6. Reflexology – stimulation of the reflexogenic zones of the neck with the help of special injections activates lymph flow and restores the immune reactivity of the mucous membranes of the oropharynx.
7. Tonsillectomy - surgical removal of the tonsils - is performed only in the case of reliable symptoms of chronic tonsillitis TAF II or in the absence of effect from a full multi-course conservative treatment of TAF I.
Surgical treatment relieves the symptoms of chronic tonsillitis from the ENT organs, but does not solve all the problems of weakened immunity. After removal of the palatine tonsils, the risk of developing bronchopulmonary pathology increases.
8. A healthy lifestyle, sufficient physical activity, regular walks in the fresh air, a balanced diet, hardening of the body (general and local), treatment of neuroses, endocrine and general diseases - all this plays a decisive role in the treatment and prevention of chemotherapy.
Chronic tonsillitis is a symptom of a decrease in the body's defenses. Timely detection and comprehensive painstaking treatment of this pathology is the prevention of cardiovascular, rheumatic, renal, pulmonary, and endocrine diseases.
Chronic tonsillitis is a situation when it is not the “plugs in the tonsils” that need to be treated, but the person.
Save the article for yourself!
VKontakte Google+ Twitter Facebook Cool! BookmarksTonsils- a collection of lymphoid tissue shaped like an almond. Their function is to recognize antigens coming from the environment and inform the immune system about them. The tonsils are part of the Waldeyer–Pirogov lymphadenoid ring surrounding the entrance to the pharynx, which consists of:
- two palatal...
- two pipe...
- pharyngeal...
- lingual tonsil.
Structure of the tonsils

Dimensions palatine tonsils vary from 7-10 mm to 2.5 centimeters. They have a smooth or slightly bumpy surface.
Parenchyma of the tonsil consists of connective tissue, between which there are a large number of lymphocytes, plasma cells and macrophages are also present. The structural unit of the tonsils is follicle, a vesicle whose walls are lined with lymphocytes. The outer surface of the tonsil is covered with stratified squamous epithelium, like the rest of the finished cavity.
Up to 20 go deep into the palatine tonsils recesses (crypts), which branch, forming large cavities lined with epithelium. The crypts contain phagocytes, microorganisms, desquamated epithelial cells, and sometimes food particles. Normally, lacunae are cleared of contents during the act of swallowing, but sometimes this process fails and purulent plugs form in the lumen of the crypts.
In the folds of the tonsils, long-term contact of external stimuli, mainly microorganisms, with the cells of the organ is ensured. It is necessary so that the immune system has time to become familiar with the pathogen and begin to secrete antibodies and enzymes to destroy them. Thus, the tonsils take part in the formation of local and general immunity.
Oral mucosa
The oral mucosa has three layers.1. Epithelial layer represented by stratified squamous epithelium. It consists of basal, spinous, granular and stratum corneum. Between the epithelial cells there are separate leukocytes. Their function is to protect against foreign bacteria and viruses. They are able to move independently and migrate to areas where inflammation develops.
2. lamina propria of the mucous membrane- a layer of connective tissue consisting of collagen and reticular fibers. Among them are:
- Fibroblasts– connective tissue cells that produce collagen fiber precursor proteins.
- Mast cells- representatives of connective tissue responsible for the chemical stability of the oral mucosa and the production of class E immunoglobulins to ensure local immunity.
- Macrophages capture and digest bacteria and dead cells.
- Plasma cells belong to the immune system and secrete 5 types of immunoglobulins.
- Segmented neutrophils- a type of white blood cell responsible for protection against infections.
The oral mucosa is pierced by ducts major and minor salivary glands. They produce enzyme-rich saliva, which has a bactericidal effect, inhibits the growth and reproduction of bacteria.
Thus, the oral cavity contains many mechanisms that protect against viruses and bacteria. A healthy body, when microorganisms enter the tonsils, copes with them without developing tonsillitis. However, when general or local immunity decreases, natural protection is disrupted. Bacteria lingering in the tonsils begin to multiply. Their toxins and protein breakdown products cause allergization of the body, which leads to the development of tonsillitis.
Causes of tonsillitis
Ways of contracting tonsillitis- Airborne. A sick or asymptomatic carrier, when coughing and talking, releases pathogens along with droplets of saliva, infecting surrounding people.
- Food. Develops when eating foods in which pathogenic microorganisms have multiplied. In this regard, the following are particularly dangerous: products with protein cream, milk and dairy products, dishes containing eggs and egg powder.
- Contact. You can become infected with tonsillitis through kissing and through household items: toothbrushes, cutlery and other utensils.
- Endogenous. Bacteria are carried into the tonsils through the blood or lymph from other sites of infection. Most often, tonsillitis occurs against the background of sinusitis, sinusitis, frontal sinusitis, otitis media, periodontitis, and caries.
- local and general hypothermia;
- acute stress reactions;
- high dust and gas content in the air;
- monotonous food with a deficiency of vitamins C and B;
- injury to the tonsils from rough food;
- lymphatic diathesis is an anomaly characterized by persistent enlargement of the lymph nodes, tonsils and thymus gland;
- disturbances in the functioning of the central and autonomic nervous system;
- chronic inflammatory processes in the oral and nasal cavities;
- reduced adaptation to environmental changes.
 1. Infection. The disease begins with the entry of pathogenic microorganisms into the tonsils. When the body's defenses are reduced, bacteria receive favorable conditions for reproduction. This leads to inflammation of the mucous membrane of the tonsils, which is expressed in their enlargement, swelling, and redness.
1. Infection. The disease begins with the entry of pathogenic microorganisms into the tonsils. When the body's defenses are reduced, bacteria receive favorable conditions for reproduction. This leads to inflammation of the mucous membrane of the tonsils, which is expressed in their enlargement, swelling, and redness.
Some bacteria enter the bloodstream. Typically, such bacteremia is short-lived. But in weakened patients, it can cause the development of purulent inflammation in other organs (abscess, otitis media).
2. Intoxication. The number of bacteria increases. Clinical manifestations at this stage are associated with the entry into the blood of bacterial enzymes that cause intoxication of the body. Signs of poisoning of the nervous system include fever, general weakness, and headache. Streptococcal enzymes streptolysin-0 (SL-O), streptokinase (SK) and hyaluronidase have a toxic effect on the heart, causing spasm of its blood vessels. Streptococcal streptolysin causes necrosis of tonsil tissue. Lymphatic cells die, and in their place voids filled with pus form.
3. Allergization. Bacterial products contribute to the formation of histamine and the development of an allergic reaction. This leads to accelerated absorption of toxins in the tonsils and increased swelling.
4. Neuroreflex lesions of internal organs. The tonsils contain many nerve receptors. They have a close reflex connection with other organs, especially with the cervical sympathetic and parasympathetic ganglia (nerve ganglia). With prolonged or chronic tonsillitis, blood circulation is disrupted and aseptic (without the participation of microorganisms) inflammation develops. Irritation of these important nerve nodes leads to disruptions in the functioning of various internal organs for the innervation of which they are responsible.
The end of tonsillitis can have two options:
1.
Destruction of microorganisms that caused tonsillitis and complete recovery.
2.
Transition of the disease into a chronic form. The immune system is not able to completely suppress the infection, and some of the bacteria remain in the folds or follicles. At the same time, there is always a focus with a “dormant” infection in the tonsils. This is facilitated by the fact that after tonsillitis, the exit from the lacunae can be narrowed by scar tissue and their self-cleaning worsens, which promotes the proliferation of bacteria. The constant presence of pathogenic microorganisms weakens the immune system and can cause autoimmune pathologies (rheumatism, rheumatoid arthritis).
Symptoms of tonsillitis
| Symptom | Development mechanism | Its manifestations |
| Fever | The reaction of the nervous system to the presence of bacterial toxins in the blood. | Acute tonsillitis - the temperature rises sharply to 38-40 degrees. Lasts 5-7 days. Chronic tonsillitis is a prolonged low-grade fever up to 37.5 degrees. |
| Inflammation of the lymph nodes | Lymph nodes trap microorganisms and their metabolic products that enter the lymphatic system. | The regional anterior cervical (closest to the tonsils) lymph nodes become inflamed. They are enlarged, not fused to the skin, and may be painful when palpated.
|
| Significant redness of the palatine arches | Bacterial toxins cause dilation of small vessels in the mucous membrane of the palatine arches. | The redness is noticeable. Edema, as a rule, is not observed.
|
| Hyperemia and swelling of the tonsils Catarrhal sore throat | Under the influence of toxins, blood vessels dilate, their permeability increases, and tissues become saturated with fluid. | Swelling and redness of the tonsils is pronounced. They can increase significantly in size.
|
| Festering follicles Follicular tonsillitis | An accumulation of pus forms in the follicles of the tonsils. | The festering follicles are visible through the epithelium. They look like yellow millet grains.  |
| Accumulation of pus in lacunae Lacunar tonsillitis | Phagocytosis actively occurs in the lacunae. Pus is formed from a mixture of bacteria, immune and epithelial cells in the cavities. | Irregularly shaped purulent plugs resemble grains of cottage cheese. They are visible in the gaps of the gaps. They often emit an unpleasant odor. A purulent plaque forms around the plugs on the surface of the tonsils, which can merge and cover its entire area.
|
| Sore throat | The tonsils are rich in nerve endings. Their irritation causes pain. | Dryness and sore throat, which sharply intensifies when swallowing. Patients have difficulty swallowing solid food. |
| General malaise | Bacterial enzymes have a toxic effect on the central and peripheral nervous system. | Pain and aches in muscles and joints, weakness, drowsiness, apathy and loss of strength. |
Diagnosis of tonsillitis
Examination by an ENT doctor
 In acute tonsillitis, patients turn to an ENT specialist with complaints of sore throat and fever. People suffering from chronic tonsillitis complain of frequent sore throats, recurring from 1 to 6 times a year. To identify their cause, a specialist conducts examination of the oral cavity - pharyngoscopy, during which he identifies a series symptoms characteristic of pharyngitis.
In acute tonsillitis, patients turn to an ENT specialist with complaints of sore throat and fever. People suffering from chronic tonsillitis complain of frequent sore throats, recurring from 1 to 6 times a year. To identify their cause, a specialist conducts examination of the oral cavity - pharyngoscopy, during which he identifies a series symptoms characteristic of pharyngitis.- Redness of the anterior and posterior palatine arches. Their edges are hyperemic and swollen.
- Swelling in the corner area, formed by the upper edges of the anterior and posterior arches.
- Redness and swelling of the tonsils.
- Enlarged tonsils. They can cover 1/3 or 1/2 of the lumen. This may indicate swelling due to tonsillitis, hypertrophic chronic tonsillitis, or anatomical features. In the absence of signs of inflammation, the size of the tonsil does not matter. It is also necessary to take into account that inflamed tonsils, with lacunae filled with pus, can be atrophic (reduced) and completely hidden behind the palatine arches.
- Purulent discharge on the tonsils may look like:
- suppurating follicles;
- purulent plugs in the lumen of lacunae or liquid pus released from them when pressed with a spatula;
- purulent plaque on the surface of the tonsils, which does not spread beyond its limits.
- Adhesion of the tonsils to the palatine arch speaks of a chronic inflammatory process. It is detected when a probe is inserted between the arch and the tonsil.
- Firm and enlarged lymph nodes.
Tonsil examination
 To detect the contents of the lacunae, the doctor lowers the root of the tongue with one spatula, and with the other, pulls back the anterior arch and slightly tilts the tonsil to the side. In this case, the lacunae are compressed and their contents come out. The inspection is carried out using a magnifying glass and a light source, which allows you to see details hidden to the naked eye.
To detect the contents of the lacunae, the doctor lowers the root of the tongue with one spatula, and with the other, pulls back the anterior arch and slightly tilts the tonsil to the side. In this case, the lacunae are compressed and their contents come out. The inspection is carried out using a magnifying glass and a light source, which allows you to see details hidden to the naked eye. Examination of lacunae is carried out with a slightly curved button probe. It can be used to take a sample of the contents for bacterial testing. A probe is inserted into the lumen of the canal to determine its depth and the presence of adhesions, which indicates chronic tonsillitis.
To identify concomitant diseases, the doctor examines the nasal cavity and auditory canals.
Biopsy for tonsillitis is rarely used, since lymphocytes are found in both healthy and inflamed tonsils. The method is used if the development of a malignant tumor is suspected.
Laboratory tests
In most cases, pharyngoscopy is sufficient to diagnose pharyngitis. However, in order to identify the pathogen and determine its sensitivity to antibiotics, a bacteriological examination of a throat smear is necessary.Swabs from the surface of the tonsils or the back of the throat
Using a sterile swab, smears of mucus are taken from the surface of the tonsils and the back wall of the pharynx. The sample is sent to the laboratory for microscopy of the material, which reveals the microorganisms that caused the disease. In the vast majority of cases, these are hemolytic streptococcus and staphylococcus. However, there are more than 30 different combinations of pathogenic, opportunistic bacteria and viruses that can cause tonsillitis.
For frequently recurring sore throats, antibiotic sensitivity test, which allows you to choose effective treatment.
However, most doctors are of the opinion that smears from the surface of the tonsils are not an informative study, since 10% of healthy people are diagnosed with streptococcus during examination, and 40% with staphylococcus.
A more informative method is counting the number of microbial cells in a smear. In acute tonsillitis, from 1.1 to 8.2 10 6 cells are detected. However, due to its labor-intensive nature, this study is rarely used.
Clinical blood test for tonsillitis:
- the ESR level increases to 18-20 mm/h;
- neutrophilic leukocytosis (increase in the number of neutrophils in the blood) up to 7-9x10 9 /l;
- band shift to the left - increase in the number of immature (band) neutrophils, the appearance of myelocytes and metamyelocytes (young).
Changes in blood tests indicate an infectious disease accompanied by an inflammatory process. In some patients, especially with chronic tonsillitis in remission, blood tests remain normal.
Determination of antibody titer to streptococcal products
Increased production of antibodies to streptolysin O over 200 IU/ml indicates the causative agent of the disease. This study is advisable to carry out only for chronic tonsillitis, since antibodies to streptolysin appear in the blood on the 7th day of illness.
Treatment of tonsillitis
Treatment of tonsillitis with medications
| Group of drugs | Mechanism of therapeutic action | Representatives | Directions for use |
| Antibiotics | They disrupt the formation of cell wall proteins, especially during division and growth. Causes the death of bacterial cells. | Ceftriaxone | Administer 1-2 g intramuscularly or intravenously once a day. |
| Ampicillin | Inside, regardless of food intake. Single dose of 0.5 g 4 times a day at regular intervals. | ||
| Amoxicillin | The dose is set individually, on average 0.5 g 3 times a day. | ||
| Sulfonamide drugs | They have a wide spectrum of action. They penetrate the bacterial cell and disrupt protein synthesis, preventing the growth and reproduction of microorganisms. | Sulfadimethoxine | Inside 1 time a day. On the first day the dose is 1-2 g, on the next 0.5-1 g. The duration of treatment is 7-14 days. |
| Sulfamonomethoxin | Take orally after meals. The first day 0.5-1 g 2 times a day. In the future, 5-1 g once a day. | ||
| Painkillers and anti-inflammatory drugs | Drugs for local treatment have an analgesic effect, reduce pain when swallowing and at rest. They also have an antimicrobial effect and reduce signs of inflammation. | Trachisan | Dissolve 1 tablet every 2 hours. |
| Neo-angin | 1 lozenge every 2-3 hours, preferably after meals. The maximum dose is 8 tablets per day. | ||
| Givalex spray | Use to irrigate the mouth 4-6 times a day. | ||
| Antiseptic solutions for rinsing | They disinfect and destroy bacteria in the oral cavity, help cleanse the lacunae of the tonsils from purulent contents. | Chlorophyllipt alcohol | The finished solution is diluted in a ratio of 1 tsp. per 100 ml of water. Repeat 4 times a day. |
| Chlorhexidine | 1 tbsp. rinse the mouth with the drug for 20-30 seconds 2-3 times a day. After the procedure, do not eat for 1.5-2 hours. | ||
| Antihistamines | Used for severe swelling of the tonsils. They help reduce swelling and reduce overall intoxication of the body. | Loratadine | 1 tablet 1 time per day. |
| Tsetrin | 1 tablet once a day. |
||
| Antipyretics | Take when the temperature rises above 38 degrees. Eliminates fever and body aches. | Paracetamol | 0.35-0.5 g 3-4 times a day after meals. |
| Ibuprofen | 400-600 mg 3 times a day after meals. |
Physiotherapeutic procedures for tonsillitis:

- Vacuum hydrotherapy of palatine tonsils– vacuum lavage of lacunae, when purulent plugs are removed under pressure. The resulting cavities are filled with an antiseptic - 0.1% hydrogen peroxide solution or antibiotic solutions. After washing, the surface of the tonsil is lubricated with Lugol's solution. The course consists of 5 procedures.
- Local ultraviolet therapy of palatine tonsils. The tonsils are irradiated with a beam of ultraviolet light according to the scheme, starting from 30 seconds to 2 minutes. There are 10 procedures prescribed per course.
- UHF. The emitter is installed on the side surface of the neck at the angle of the lower jaw. Session duration is 7 minutes. The course of treatment is 10-12 procedures.
Nutrition and lifestyle for tonsillitis
For acute tonsillitis (sore throat) physical activity is contraindicated. Excessive activity increases the load on the heart and increases the risk of complications. Therefore, it is advisable to adhere to bed rest for the entire treatment period.For chronic tonsillitis in remission It is advisable for patients to move more and be in the fresh air for at least 2 hours a day. Physical inactivity worsens the immune system. It has been proven that with insufficient physical activity, the local protective properties of the oral mucosa and tonsils worsen by 5-8 times. Therefore, regular exercise significantly reduces the number of exacerbations of tonsillitis.
- Avoid dusty and smoky air.
- Stop smoking.
- Humidify the indoor air. Humidity should be at least 60%.
- Toughen up. Contrast showers, cold rubdowns, and dousing with cold water are recommended daily.
- Spa therapy on the sea coast. Swimming, sunbathing and rinsing with sea water increase general and local immunity. Duration of treatment is 14-24 days.
- Follow a daily routine and allocate enough time for rest. Don't overwork yourself and avoid stress.
Table No. 13 is recommended for patients with acute and exacerbation of chronic tonsillitis. This diet is aimed at strengthening the body's defenses and quickly eliminating toxins.
Culinary processing - boiling in water or steaming. This helps ensure that the dishes are as gentle as possible. The mucous membrane of the mouth and pharynx should not be injured mechanically, thermally or chemically, therefore all dishes should be liquid or semi-liquid, temperature 15-65 degrees. Hot, spicy and sour foods are excluded.
During illness, frequent meals in small portions 5 times a day are necessary. It is advisable to take food during those hours when the temperature drops and appetite appears.
It is necessary to increase fluid intake to 2.5 liters per day. This reduces the concentration of toxins in the body and promotes their elimination in the urine.
 Recommended Products:
Recommended Products:
- Wheat bread baked yesterday.
- Meat or fish soups. Not rich, low-fat - for this, drain the first water when cooking meat. Vegetables, pasta and cereals are added to soups. Since it is difficult for patients to swallow, soups are pureed or crushed in a blender.
- Steamed lean meats, poultry and fish. Steam cutlets, meatballs, and meatballs are also recommended.
- Fermented milk products, fresh low-fat cottage cheese, mild cheese. Sour cream is used only for seasoning dishes.
- Semi-liquid, viscous porridge from cereals.
- Vegetable side dishes: mashed potatoes, stew, vegetable caviar.
- Fresh fruits and berries, not hard or sour. Jam, compotes, jelly, juices diluted with water 1:1.
- Honey, marmalade, jam.
- Drinks: weak tea and coffee, rose hip decoction.
- Baking, rye bread.
- Fatty fish and meats, broths made from them.
- Smoked meats, canned food, salted fish.
- Barley and pearl barley, millet.
- Cream, whole milk, sour cream, fatty cheeses.
- Products that increase gas formation: cabbage, legumes, radishes, radishes.
- Spices, hot seasonings.
- Strong tea, coffee.
- Alcoholic drinks.
When is it necessary to remove tonsils?
 According to the modern approach, doctors try to avoid removing the tonsils, since they perform an important protective function - they recognize the infection and delay it. The exception is cases when a chronic inflammatory focus threatens to cause serious complications. Based on this, surgery to remove tonsils (tonsillectomy) is performed strictly according to indications.
According to the modern approach, doctors try to avoid removing the tonsils, since they perform an important protective function - they recognize the infection and delay it. The exception is cases when a chronic inflammatory focus threatens to cause serious complications. Based on this, surgery to remove tonsils (tonsillectomy) is performed strictly according to indications. tuberculosis in the active phase. In recent years, cauterization with liquid nitrogen, laser, and electrocoagulation of damaged areas of the tonsils has been used as an alternative to tonsil removal. In this case, the organ gets rid of the source of infection and continues to perform its functions.
Prevention of tonsillitis
The main task of preventing tonsillitis is to prevent a decrease in immunity and avoid infection.What is needed for this?
- Lead a healthy lifestyle. This concept includes proper nutrition, physical activity and proper rest. Food should be rich in easily digestible proteins, vitamins and microelements. In this case, it helps strengthen the body's natural defenses.
- Will be tempered. You need to start hardening by pouring water at room temperature or swimming in an open pond for 3-5 minutes. Gradually, the water temperature is reduced and the time spent in the reservoir is increased.
- Maintain good hygiene: do not use other people’s toothbrushes, do not drink from the same cup, wash dishes thoroughly. Provide separate equipment for the patient.
- Restore impaired nasal breathing. To do this, you need to contact an ENT specialist.
- Monitor the condition of the mouth and teeth. Visit the dentist at least once a year.
- Gargle 2 times a day with diluted colanchoe juice (1 tsp per glass of water), infusions of chamomile or calendula. This recommendation will help people who often experience a sore throat.
- Massage of the front of the neck performed with stroking movements from the chin to the earlobes, from the upper jaw to the collarbones. Massage improves blood circulation and lymph flow, helps increase local immunity. It is recommended to perform it before going outside or after hypothermia.
- Contact with patients with sore throat. If possible, isolate the patient from other family members.
- Crowded places, especially during periods of epidemics, when there is a high probability of becoming infected.
- Overheating and hypothermia, as this entails a decrease in immunity.
- Smoking, consumption of strong alcoholic drinks, burning the mucous membrane of the throat.
Tonsillitis is an inflammatory process that occurs in the area of the palatine tonsils and is characterized by a long-lasting course. Tonsillitis, the symptoms of which are also defined as the more common name for the disease “angina,” consists of pathological changes in the oropharynx that are similar to each other, but differ in the characteristics of their own etiology and course.
General description
Sore throat has been known since ancient times of ancient medicine, and most often this term indicates the relevance of various types of painful conditions concentrated in the throat area and having similar symptoms. Meanwhile, the reasons that provoked tonsillitis inherently determine for the disease an absolute difference in the varieties of its forms. Taking this fact into account, all current variants of this disease can be divided into three separate categories: primary tonsillitis, specific tonsillitis, secondary (or symptomatic) tonsillitis.
Primary sore throats
Primary sore throats are an infectious acute disease characterized mainly by its own streptococcal etiology, as well as a relatively short course of fever, intoxication and inflammatory changes occurring in the tissues of the pharynx (mainly in the tonsils and lymph nodes located near them).
The danger of this form of the disease lies in the fact that it begins the development of autoimmune processes, the absence of treatment of which can cause the development of acute forms and, in turn, lead to serious damage to the heart and kidneys.
Most often, tonsillitis appears as a result of exposure to a beta-hemolytic pathogen, and a similar course of the disease is observed in about 90% of cases. In 8% of morbidity cases, tonsillitis develops due to exposure, in some cases combined with streptococcus.
It is extremely rare that the causative agent is Haemophilus influenzae, Corynebacterium or Streptococcus pneumoniae. In the case of tonsillitis, the source of the pathogen is a patient with one or another disease in its acute form and a carrier of microorganisms of pathogenic flora.
The main route of infection with the disease is through airborne droplets, which is extremely common in large groups, as well as as a result of close contact with a sick person. Infection can also occur as a result of consuming products previously contaminated with staphylococcal infection (compote, milk, minced meat, salad, etc.).
Regarding susceptibility to the disease, it can be noted that it is not the same for each patient, being determined to a large extent by the condition inherent in the local immunity of the tonsil area. So, the lower the immunity, the correspondingly higher the risk of disease.
This risk also increases as a result of overwork, hypothermia, and exposure to other unfavorable factors. The incidence of primary tonsillitis is characterized by correspondence to certain seasons, namely spring and autumn. Tonsillitis is observed in both children and adults.
Secondary tonsillitis
Secondary tonsillitis are an acute type of inflammation, concentrated in the area of the components of the pharyngeal lymphatic ring, which mainly concerns the palatine tonsils. This type of disease is caused by a specific systemic disease.
The development of secondary sore throats occurs as a result of a number of infectious diseases, which include herpes, etc.
A separate group includes those sore throats that develop against the background of current and relevant symptoms for patients.
Acute tonsillitis: main features and forms of the disease
The lymphoid tissue of the oropharynx region acts as the entry gate for the disease; it is in it that the formation of the primary focus of the inflammatory process occurs. Predisposing factors to the development of acute tonsillitis include local hypothermia, increased dryness in the air, gas and dust in the atmosphere, decreased immunity, nasal breathing disorders, hypovitaminosis, etc.
In frequent cases, the development of sore throat occurs as a result of the patient’s transmission of the pathogen, the action of which is aimed at reducing the protective functions characteristic of the epithelial cover, this, in turn, facilitates the process of streptococcal invasion.
Based on the nature of the lesion and its depth, the following types of tonsillitis are determined:
- necrotizing tonsillitis.
Of the listed forms of tonsillitis, the mildest course is observed in the catarrhal form of the disease, and the most severe in its necrotic form.
Based on the characteristic severity, tonsillitis can be mild, moderate or severe. The severity of this disease is determined by the severity of changes on a general and local scale, and it is the general manifestations that are decisive in determining this criterion.
Acute tonsillitis: symptoms
The total duration of the incubation period relevant for this disease is about 10 hours to three days. The onset of manifestations of the disease is characterized by severity, the main ones being high fever and chills, as well as severe pain felt when swallowing. In addition, there is an increase in lymph nodes and their soreness. The nature of the severity of fever accompanying tonsillitis, as well as the nature of the pharyngoscopy picture in combination with intoxication, is determined based on the form of the disease.
Symptoms of catarrhal tonsillitis
A characteristic feature of this form of the disease is the superficiality of the lesion in the tonsil area. Intoxication manifests itself moderately, the temperature in patients is low-grade.
A blood test determines the absence of changes in it or the insignificance of this phenomenon. Pharyngoscopy reveals diffuse and fairly bright hyperemia, which captures the hard and soft palate, as well as the pharynx (its posterior wall). Somewhat less often, hyperemia during tonsillitis is limited only to the palatine arches and tonsils. A characteristic enlargement of the tonsils occurs due to swelling and infiltration.
The duration of the disease is about two days, after which there is a gradual subsidence of the inflammatory processes of the pharynx, or, conversely, another form of tonsillitis begins to develop (follicular or lacunar).
The course of follicular and lacunar tonsillitis is characterized by a much more pronounced clinical picture. Thus, the temperature in these cases rises to 40 degrees, and manifestations characteristic of intoxication (headache, weakness, pain in the joints, muscles and heart) also become pronounced.
Catarrhal tonsillitis (acute tonsillopharyngitis) is a pathological process caused by pathogenic microflora and affecting the upper layers of the mucous membrane of the throat. This form, according to medical terminology, is also called erythematous. Of all the forms of sore throat, this one is considered the mildest, but this does not mean at all that it does not need to be treated. Only a qualified doctor can correctly tell how to treat catarrhal tonsillitis after a comprehensive diagnosis. It is also worth noting that treating an illness does not always require the use of antibacterial drugs.
Sore throat is an illness of an infectious nature, as a result of the progression of which acute inflammation of the palatine tonsils and other lymphoid formations of the pharynx occurs. The following pathogenic microorganisms can provoke the development of pathology: viruses, bacteria and fungi. In the medical literature, this condition is also called acute tonsillitis. It is worth noting that this is a fairly common disease that can begin to progress in both adults and children.
Chronic tonsillitis is a very common ENT disease that occurs as a result of frequent inflammation of the tonsils. Chronic tonsillitis in adults occurs in 4-30% of cases. This prevalence of the disease, combined with the possible development of complications, indicates the danger of the disease and the relevance of its early treatment.
What is tonsillitis
Tonsillitis is called inflammation in the area of the tonsils, that is, in the area of the palatine tonsils, which occurs in acute and chronic forms.

Acute tonsillitis is popularly called - it occurs in a recurrent form, in which inflammation of the pharyngeal mucosa occurs sharply and frequently. The chronic form of the disease is sluggish - in it, inflammation can last up to three weeks with mild symptoms.
Chronic tonsillitis is more dangerous because can manifest itself several times a year, without causing any particular inconvenience or discomfort at first. Therefore, many patients at first do not even try to identify the cause of the manifestations of the disease, believing that everything will go away on its own. However, after some time, the symptoms begin to increase, and then you have to seek the help of a specialist and begin long and unpleasant treatment.
Pay attention! The acute form of tonsillitis is called.
If treatment for tonsillitis is not started on time, serious complications may develop, which include:
- Rheumatism;
- Glomerulonephritis (autoimmune kidney disease);
- Peritonsillar abscess;
- Chronic intoxication of the immune system.
Chronic tonsillitis, the symptoms of which do not always make themselves felt, can cause the development of various pathological processes in almost all systems and organs. Due to disturbances in the neuro-reflex and endocrine regulation of the body, depression, menstrual irregularities, Meniere's syndrome, etc. can occur.
Chronic tonsillitis is very dangerous for expectant mothers: during pregnancy, many women, faced with manifestations of the disease, do not attach due importance to them, and therefore do not begin treatment on time. However, the disease can seriously affect the baby’s health, because tonsils, which create a barrier to infection, become inflamed during tonsillitis and create a risk of microbes penetrating through the blood to the baby.
Therefore, at the first symptoms of the disease, pregnant women should immediately seek medical help. Untreated tonsillitis can lead to premature birth and cause severe pain.
Why does tonsillitis appear?
Inflammation of the palatine tonsils is based on an infectious lesion caused by pneumococci, Candida fungi and other pathogenic microorganisms. Many such microorganisms live on the human tonsils. Healthy tonsils cope with pathogenic bacteria, but inflamed tonsils do not have enough strength for such a fight.
Pay attention! The causes of tonsillitis are pathogenic bacteria that “live” on the human tonsils.
The main reasons for the transition of tonsillitis to a chronic form:
- Untreated sore throat. Often the patient stops treatment and antibiotics as soon as the temperature drops and the sore throat subsides. In fact, the disease only subsides for a while and, if you do not completely stop taking antibiotics and do not strengthen it with vitamins, tonsillitis will return with renewed vigor.
- Frequent pharyngitis. The patient often does not pay due attention to the appearance of pharyngitis, not even bothering to consult a doctor when it occurs. As a result, a pathological process develops, and the slightest weakening and fatigue lead to the appearance of chronic tonsillitis.
Provoking factors for tonsillitis in adults:
- Stress;
- Reduced immunity;
- Regular hypothermia;
- Having bad habits;
- Frequent overwork;
- Incorrect diet with a reduced composition of vitamins;
- Chronic pathologies of the digestive and respiratory organs;
- Hereditary predisposition;
- Deviation of the nasal septum;
- Inflammatory processes of ENT organs (, adenoids);
- Caries;
- Formation of polyps in the nasal septum.

Also, the appearance of tonsillitis can be caused by allergic reactions, which not only affect the progression of the disease, but also often cause complications.
Signs and symptoms
Chronic tonsillitis itself usually does not manifest itself in any way - you can often find out about the presence of the disease only during an exacerbation, when a diagnosis of “angina” is usually made.
Symptoms of chronic tonsillitis
Manifestations of the disease in chronic form are similar in symptoms to other diseases, and therefore they are not always paid attention to. The first alarming symptoms indicating the occurrence of tonsillitis may be the appearance of frequent headaches, decreased performance, weakness and general malaise. Such symptoms are associated with intoxication of the body by waste products of bacteria that have reached the tonsils.
Another, more pronounced sign is the appearance of a feeling of a foreign object in the throat. This phenomenon is explained by blockage of the palatine tonsils with large plugs, which is usually accompanied by the occurrence of bad breath.
Tonsillitis most often manifests itself with the following symptoms:
- in the throat;
- Enlarged and painful lymph nodes;
- Pain when swallowing"
- Increased temperature;
- Coughing up pus.
Unpleasant symptoms can appear from almost all human organs and systems, because pathogenic bacteria can penetrate from the tonsils to any place in the body.
Additional symptoms:
- Pain in the joints;
- Allergic skin rashes that cannot be treated;
- "Aches in the bones"
- Mild cardiac colic, disruptions in the functioning of the cardiovascular system;
- Pain in the kidney area, disruption of the genitourinary system.

Symptoms of acute tonsillitis
Acute tonsillitis manifests itself depending on the form in which the disease occurs.
Catarrhal form manifests itself with the following symptoms:
- Migraine;
- Pain when swallowing;
- General weakness;
- Temperature rise to 38 degrees (or higher);
- Dry and sore throat.
Follicular form characterized by the following features:
- Chills;
- Loss of appetite;
- The appearance of suppuration on the tonsils;
- Severe headaches;
- Swelling of the tonsils and surrounding tissues;
- Loss of appetite;
- Increased sweating;
- Feeling of aches and general weakness.
Phlegmonous form appears as follows:
- Severe headaches;
- Enlarged lymph nodes in the neck;
- Sharp pain in the throat;
- Bad breath;
- General weakness and loss of appetite;
- The appearance of nasality;
- The occurrence of chills;
- Increased salivation;
- High temperature (over 39 degrees).
Tonsillitis caused by viruses is accompanied by the appearance of herpetic blisters on the tonsils.
Diagnostics
An otorhinolaryngologist or an infectious disease specialist can carry out an accurate diagnosis of the disease, as well as identify the degree of its activity, stage and form, based on general and local manifestations, objective symptoms, amnestic data, and laboratory indicators.
Tonsillitis manifests itself most clearly during exacerbations - then it is best to carry out diagnostics.
The doctor carefully analyzes the patient’s complaints, after which he performs pharyngoscopy - examination of the palatine tonsils and adjacent areas. Upon examination, you can detect the following signs of tonsillitis (see photo):

- Swelling and thickening of the edges of the palatine arches;
- Fusion of the arches of the palate with the tonsils (and/or with the triangular fold);
- Loosening of tonsils;
- Increase in regional nodes;
- Purulent plaque on the tonsils;
- Redness of the anterior palatine arches.
Usually, to establish a diagnosis, a thorough analysis of the patient’s complaints and pharyngoscopy is sufficient, but sometimes the doctor may prescribe additional tests: a general clinical blood test, a bacteriological study of the secretions of the palatine tonsils, a biochemical blood test.
Treatment methods
Treatment of tonsillitis can be carried out in two ways: conservative and surgical. If 30 years ago specialists tried not to treat tonsillitis, but immediately resort to removing the tonsils, now doctors mainly use conservative treatment using modern medical technologies and medications.
Important! A prerequisite for treating tonsillitis is bed rest along with a gentle diet and plenty of fluids.
Conservative treatment
Chronic tonsillitis should be treated comprehensively - twice a year during the period of remission.
How to treat chronic tonsillitis in adults:
- Sanitation of foci of infection. Includes timely treatment of nasal diseases, dental diseases and other pathologies that are predisposing factors in the occurrence of tonsillitis. If necessary, surgical intervention is performed: straightening the nasal septum, removing adenoids, etc.
- Local treatment. The lacunae of the palatine tonsils are regularly cleansed from pathological deposits. The tonsils are washed with a solution of chlorophyllipt, furatsilin,. It is better not to cleanse yourself, so as not to damage the mucous membrane of the throat.
- Drug treatment. In some cases, antibiotics are prescribed for tonsillitis in adults: macrolides, penicillins, cephalosporins. This treatment is most often prescribed for purulent forms of tonsillitis, and the drugs are selected individually - depending on the stage of the disease, symptoms and sensitivity of microorganisms to antibiotics. To reduce allergic reactions, medications are prescribed in parallel.
- Strengthening the immune system. You should pay attention to proper rest, nutrition, and hardening activities. If necessary, prescribe the use of plant (aloe, eleutherococcus, ginseng) or synthetic (interferon) origin.
- Physiotherapeutic procedures. Physiotherapeutic procedures have a good effect in the treatment of tonsillitis: ultrasound, microwave, UHF, ultraviolet irradiation, electrophoresis, laser therapy. Physiotherapy is contraindicated in the presence of cancer, pregnancy, and decompensated diseases of internal organs.
When treating chronic tonsillitis, it is possible to take painkillers (for example, Nurofen) to relieve pain. For minor pain, there is no point in using such medications.
The drugs help reduce swelling of the tonsils and pharyngeal mucosa. The best-proven drugs are Telfast and Zyrtec - they are safer, have a long-lasting effect and do not have a pronounced sedative effect.

Treatment of tonsillitis in adults at home is necessarily accompanied by the use of local antiseptic drugs in the form of lozenges, sprays, solutions (Faryngosept, Hexoral).
Surgical treatment
Surgical methods are used to treat tonsillitis in a number of cases:
- In the absence of a therapeutic effect with conservative methods;
- In case of development of an abscess against the background of tonsillitis;
- When tonsillogenic sepsis occurs;
- If malignant pathologies are suspected.
Surgical methods involve the removal of tonsils (most often on both sides) in two main ways:
- Tonsiectomy – complete removal of tonsil tissue.
- Tonsillotomy is a partial excision of the tonsils.

Such operations, as a rule, take place without complications. After surgery, the patient is prohibited from eating and talking for 24 hours.
The operation cannot be performed under the following conditions:
- Cardiovascular pathologies;
- in the uncompensated stage;
- Diseases of the hematopoietic system;
- Arterial hypertension, in which a hypertensive crisis and intense bleeding during surgery are possible.
In some clinics, it is currently possible to remove tonsils using low temperatures - the cryomethod.
Traditional methods
Treatment of tonsillitis with folk remedies is more popular than conservative and surgical treatment methods. Traditional medicine has hundreds of recipes that help eliminate unpleasant symptoms of the disease and get rid of the disease as quickly as possible.
Traditional methods help to externally influence the palatine tonsils and stimulate the internal atmosphere of the body to fight the disease. External remedies include infusions and decoctions for rinsing, compresses and poultices for the neck area, healing pastes for tonsils. Internal remedies include decoctions, teas, tinctures, and inhalations.

An excellent and effective remedy for the treatment of tonsillitis is the use of hot liquids during the period of illness: various teas, herbal decoctions, broths, hot milk. All these methods will help ease the course of the disease and reduce inflammation in the throat.
Prevention
Preventive measures for the occurrence of tonsillitis include measures to prevent the occurrence of tonsillitis and proper treatment of the disease:
- Sanitation of the nasopharynx and oral cavity;
- Prevention of colds (especially during seasonal exacerbations);
- Limiting contact with those who have recently been ill or are sick;
- Measures to strengthen the immune system: regular exercise, proper nutrition, hardening, walks in the fresh air;
- Avoiding overheating and hypothermia.
Getting proper rest, avoiding stress and following a daily routine will help prevent disease and strengthen the body's defenses.
Diagnosis of tonsillitis: questions to the doctor
When treating tonsillitis, questions often arise that only a qualified specialist can answer. It is not always possible to consult a doctor with a question of interest, so we provide a list of the most common questions with answers from otorhinolaryngologists.
Can tonsillitis be cured with antibiotics? Can. But chronic tonsillitis outside the acute phase is best treated by other means - local therapy and physiotherapeutic procedures.
Do sprays and gargles help treat tonsillitis? Rinsing and using a spray only dulls the symptoms; the disease cannot be cured with these procedures alone, because the infection is deep in the tonsils. The procedures are used in complex therapy along with drug treatment, rinsing, etc.
Should folk remedies be used to treat tonsillitis? Folk remedies in combination with basic treatment methods give good results, so it makes sense to use them as immunostimulating and analgesic therapy.
The doctor diagnoses “chronic tonsillitis”, but there are no symptoms. Does this mean the doctor is wrong? The diagnosis is made on the basis of comprehensive data: medical history, local signs of the disease, laboratory tests. If symptoms do not appear, this does not mean that you should not ignore the doctor’s prescriptions and recommended treatment.





 Nature calendars series “The world around us”
Nature calendars series “The world around us”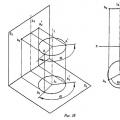 Methods for converting a complex drawing Method for replacing projection planes
Methods for converting a complex drawing Method for replacing projection planes Why do you dream about a closet - interpretation of sleep
Why do you dream about a closet - interpretation of sleep